 On behalf of the Acus team, we give a warm welcome to our fifth cohort of military physicians and clinicians, the Class of 2019-2020! On Friday, our latest class of students began their training in comprehensive Acus medical acupuncture in North Las Vegas, Nevada.
On behalf of the Acus team, we give a warm welcome to our fifth cohort of military physicians and clinicians, the Class of 2019-2020! On Friday, our latest class of students began their training in comprehensive Acus medical acupuncture in North Las Vegas, Nevada.
The 27 students hail from all five Family Medicine Residencies in the U.S. Air Force, based at Eglin AFB (Florida), Nellis AFB (Nevada), Offutt AFB (Nebraska), Scott AFB (Illinois), and Travis AFB (California). We also welcome students from both the Southern Nevada VA and the Salt Lake City VA.
Study hard and get ready for the exciting journey ahead!


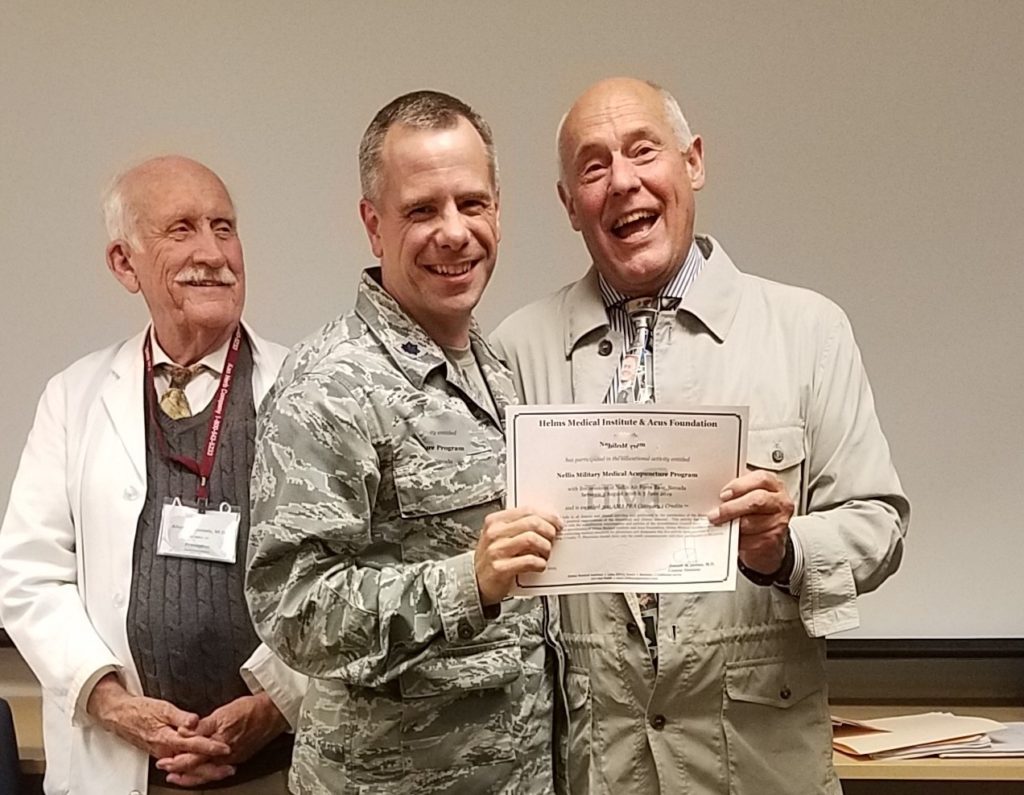 Acus Founder, Dr. Joseph Helms, right, presents a certificate to a course graduate, center, at commencement in early June. Preceptor Allen McDaniels, far left, looks on with a smile.
Acus Founder, Dr. Joseph Helms, right, presents a certificate to a course graduate, center, at commencement in early June. Preceptor Allen McDaniels, far left, looks on with a smile.


